Understanding and Managing 3rd Degree Vaginal Tears: A Guide for New Parents
Bringing a new life into the world is a beautiful, albeit challenging, experience. But sometimes, the journey of childbirth can come with unexpected hurdles, such as a 3rd degree vaginal tear. First off, it’s important to know that you are not alone, and such conditions are manageable with the right care and support. This guide is here to embrace you with necessary information, comfort, and reassurance every step of the way.
What is a 3rd Degree Vaginal Tear?
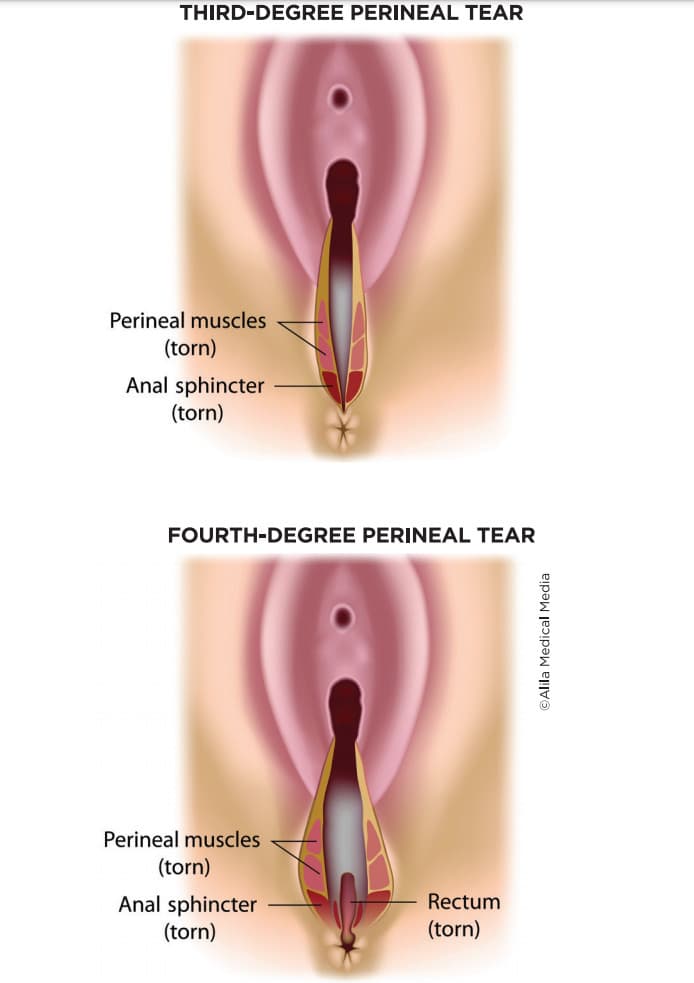
During the delivery of a baby, especially a vaginal delivery, the mother’s body undergoes significant stress. A 3rd degree vaginal tear is a type of perineal tear that extends into the muscles that surround the anus (the anal sphincter). These types of tears, though not as common as first or second-degree tears, are more significant and require attentive medical intervention.
How Does a 3rd Degree Vaginal Tear Occur?
Several factors can increase the likelihood of experiencing a more severe perineal tear, including delivering a larger baby, a prolonged second stage of labor, or the need for an assisted delivery, such as with forceps or a vacuum. It’s also worth noting that every woman’s body is unique, and even with prevention measures, tears can happen.
Immediate Treatment and Healing
Let’s take a deep breath, because there are established protocols for treating a 3rd degree tear. It’s a buzz of activity, but you can rest assured that healthcare professionals are trained for exactly these situations. Here’s what typically happens:
- Assessment: Following the delivery, your healthcare provider will assess the tear to determine its severity. Be prepared for them to inform you clearly about the extent of the tear and what the next steps will be.
- Repair: 3rd degree tears are repaired in an operating theatre to ensure a sterile environment and the best possible outcome. The tear is generally sutured under regional anesthesia.
- Recovery: Post-operative care includes pain management, instructions for personal hygiene, and advice on activity levels to allow you to heal and bond with your baby.
Now, as a new parent, you might wonder about the road to recovery and how to care for yourself while adjusting to life with your little one. Here’s a snippet to get you started:
Postpartum Care and Recovery
The physical and emotional recovery from a 3rd degree vaginal tear is paramount. You can expect your healthcare team to provide detailed guidance on how to manage pain, avoid infections, and promote healing. Some components of care include:
- Medication for pain relief
- Guidance on keeping the area clean and dry
- Instructions on how to use ice packs to reduce swelling
- Recommendations on when and how to resume physical activities
- Advice on dietary adjustments to prevent constipation, which can strain the repair
Remember that your follow-up appointments are vital. They provide an opportunity for your medical team to ensure your healing process is on track and offer you a platform to address any concerns or ask questions.
As you navigate this sensitive period, it’s also crucial to acknowledge the emotional impact such a birth injury can have. Don’t hesitate to reach out for psychological support if you find yourself overwhelmed. Loving care, patience, and open communication with your support system and healthcare providers will all play essential roles in your recovery journey.
Don’t forget, the resilience of the human body and especially the warrior spirit of mothers is phenomenal. With time and proper care, you will heal. Stick with us as we delve deeper into how to manage life post-tear, with practical tips to ease your day-to-day and wisdom to support your emotional wellbeing. Stay tuned for more supportive insights on your path to recovery.
5 Key Things Parents Should Know in Preparing for a 3rd Degree Vaginal Tear
1. Understand the Risks and Causes
Being informed about what could potentially lead to a 3rd degree tear is crucial. Discuss with your healthcare provider your individual risk factors such as your baby’s size, your pelvic anatomy, and your childbirth history. This awareness can help you make informed decisions about your delivery plan.
2. Learn About Prevention Strategies
While not all tears can be prevented, there are strategies that might reduce the risk. These include perineal massage during pregnancy, controlled pushing during delivery, and the use of warm compresses to soften the perineum. Ask your healthcare provider about exercises and techniques that can strengthen your pelvic floor and tissues.
3. Make a Birth Plan, but Stay Flexible
Creating a birth plan is a proactive step, but it’s important to be flexible. In some cases, interventions such as episiotomies are performed to prevent more significant tears. Being mentally prepared for changes in your delivery plan will make any necessary decisions less stressful.
4. Assemble a Support Team
Postpartum recovery requires physical and emotional support. Assembling a team that includes your partner, family members, friends, or even a postpartum doula can prove invaluable. Ensure your team understands the possibility of needing extra help if a severe tear occurs.
5. Be Proactive with Postpartum Care Supplies
Having the right supplies at home can make a huge difference. Stock up on essentials like pain relievers, stool softeners, ice packs, and hygiene products specially designed for postpartum care. Seamless access to these supplies will allow you to focus on recovery and bonding with your baby.
Comprehensive Post-Tear Management
Life after experiencing a 3rd degree tear might seem daunting, but rest assured, with a supportive care plan, recovery is absolutely possible. Communicate openly with your healthcare provider about the best pain management techniques for you, and remember that attending to your wound care is just as vital as tending to your newborn.
Ensuring a nutritious diet rich in fiber can soften stools and prevent constipation, which is incredibly important as straining can impede tear healing. Furthermore, scheduling time for rest and allowing your body to heal without overexerting yourself is essential for a smooth recovery.
It may be challenging at first, but gentle walks and eventually pelvic floor exercises (when cleared by your healthcare provider) can aid your physical recovery and strengthen your muscles. Additionally, staying hydrated can promote healing and maintain your overall health, which is particularly critical when you’re breastfeeding.
Lastly, keep in mind that emotional healing is just as important as physical recovery. Finding a community of new mothers, speaking to a counselor, or just sharing your experiences with your partner or friends can make a considerable difference in how you cope with the postpartum period.
Remember, each day you are getting stronger, your body is healing, and you are getting more adept at caring for your little one. Embrace each small victory and know that you’re doing an incredible job. This period is just one chapter in the rewarding story of parenthood.
See more great Things to Do with Kids in New Zealand here. For more information see here
Disclaimer
The articles available via our website provide general information only and we strongly urge readers to exercise caution and conduct their own thorough research and fact-checking. The information presented should not be taken as absolute truth, and, to the maximum extent permitted by law, we will not be held liable for any inaccuracies or errors in the content. It is essential for individuals to independently verify and validate the information before making any decisions or taking any actions based on the articles.




